Possible Treatment of a Broken Foot
 A common reason a broken foot may occur can be from falling off of a ladder, or it may become injured from participating in sporting events. The bones that are located between the toes and the ankle are referred to as the metatarsals. They can be prone to stress fractures, which typically happen from overuse. The average healing time for a broken foot is generally six to twelve weeks. Many daily activities are able to be completed as the healing process occurs when a walking boot or cast is worn. For more severe fractures, it may take longer if surgery is required. If you have pain in your feet as a result of either a fall or something else, it is advised that you consult with a podiatrist.
A common reason a broken foot may occur can be from falling off of a ladder, or it may become injured from participating in sporting events. The bones that are located between the toes and the ankle are referred to as the metatarsals. They can be prone to stress fractures, which typically happen from overuse. The average healing time for a broken foot is generally six to twelve weeks. Many daily activities are able to be completed as the healing process occurs when a walking boot or cast is worn. For more severe fractures, it may take longer if surgery is required. If you have pain in your feet as a result of either a fall or something else, it is advised that you consult with a podiatrist.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Brian D. Jackson, DPM from Neuhaus Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Possible Causes of Bunions
 A bump that extends on the side of the big toe may indicate a bunion. It is considered to be a deformity, and a common cause can be from wearing shoes that do not have adequate room for the toes to move freely in. Additionally, genetics can play a significant role in developing a bunion. Mild relief may be found when larger shoes are purchased, and it may help to wear a protective covering over the top of the bunion. In severe cases, orthotics can be prescribed, and therapy techniques may be suggested. If you notice a bony protrusion on the side of the big toe, it may be a bunion, and it is strongly suggested that you seek treatment from a podiatrist.
A bump that extends on the side of the big toe may indicate a bunion. It is considered to be a deformity, and a common cause can be from wearing shoes that do not have adequate room for the toes to move freely in. Additionally, genetics can play a significant role in developing a bunion. Mild relief may be found when larger shoes are purchased, and it may help to wear a protective covering over the top of the bunion. In severe cases, orthotics can be prescribed, and therapy techniques may be suggested. If you notice a bony protrusion on the side of the big toe, it may be a bunion, and it is strongly suggested that you seek treatment from a podiatrist.
If you are suffering from bunion pain, contact Brian D. Jackson, DPM of Neuhaus Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
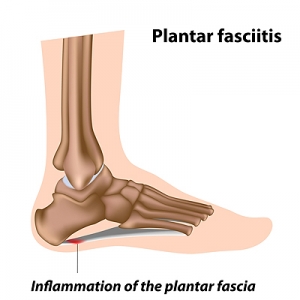
Can Sudden Weight Gain Cause Plantar Fasciitis?
 Research has indicated the condition known as plantar fasciitis is the most common cause of heel pain. The majority of patients notice the pain and discomfort is worse in the morning, and can be felt when the first steps are taken. Plantar fasciitis can occur when the plantar fascia becomes inflamed. This is the portion of tissue that is located on the sole of the foot, and its function is to connect the heel to the toes. When this condition develops, the pain may be managed when appropriate foot and calf stretches are performed. It can be caused by a variety of reasons. These can include wearing shoes that do not fit properly, and standing for extended periods of time throughout the day. Additionally, it may occur as a result of beginning a new running regime, or if there has been a significant weight gain. If you have heel pain, it is suggested that you consult with a podiatrist who can properly diagnose and treat plantar fasciitis.
Research has indicated the condition known as plantar fasciitis is the most common cause of heel pain. The majority of patients notice the pain and discomfort is worse in the morning, and can be felt when the first steps are taken. Plantar fasciitis can occur when the plantar fascia becomes inflamed. This is the portion of tissue that is located on the sole of the foot, and its function is to connect the heel to the toes. When this condition develops, the pain may be managed when appropriate foot and calf stretches are performed. It can be caused by a variety of reasons. These can include wearing shoes that do not fit properly, and standing for extended periods of time throughout the day. Additionally, it may occur as a result of beginning a new running regime, or if there has been a significant weight gain. If you have heel pain, it is suggested that you consult with a podiatrist who can properly diagnose and treat plantar fasciitis.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Brian D. Jackson, DPM from Neuhaus Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
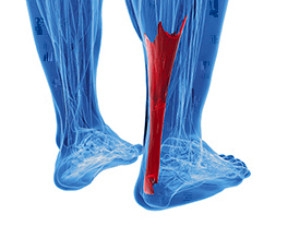
Possible Treatments for an Achilles Tendon Injury
 The Achilles tendon connects the heel to the calf muscles. It is located in the back of the leg, near the foot, and is responsible for the ability to point and flex the foot. An injury can cause the Achilles tendon to become ruptured or injured, and this generally causes severe pain and discomfort. Some of the symptoms that many patients can experience include sharp pain at the time of the injury, bruising, swelling, and it is often difficult to walk. This type of injury can happen as a result of participating in running and jumping movements, or if a new activity begins suddenly. Effective treatments can include wearing a brace or cast as the healing process occurs, and in severe tears, surgery may be necessary. If you have pain in your calf, it is strongly advised that you speak to a podiatrist as quickly as possible who can treat an Achilles tendon injury.
The Achilles tendon connects the heel to the calf muscles. It is located in the back of the leg, near the foot, and is responsible for the ability to point and flex the foot. An injury can cause the Achilles tendon to become ruptured or injured, and this generally causes severe pain and discomfort. Some of the symptoms that many patients can experience include sharp pain at the time of the injury, bruising, swelling, and it is often difficult to walk. This type of injury can happen as a result of participating in running and jumping movements, or if a new activity begins suddenly. Effective treatments can include wearing a brace or cast as the healing process occurs, and in severe tears, surgery may be necessary. If you have pain in your calf, it is strongly advised that you speak to a podiatrist as quickly as possible who can treat an Achilles tendon injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Brian D. Jackson, DPM of Neuhaus Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Why Do Cracked Heels Form?
 Having dry skin is one of the many factors that can result in the formation of cracked heels. Those who have biomechanical issues that increase the pressure put on the heel, may be more likely to experience cracked heels. Being obese can also create an increase in pressure put on the heels, as the feet are responsible to carry the extra weight. This causes a loss of suppleness in the pads of the feet. Due to this lack of flexibility and increased pressure, cracks and deep fissures can form on the heels. Wearing open back shoes can also be a risk factor for developing cracked heels, as these types of shoes may cause the fat pads in the heel to expand sideways, creating cracks. Certain skin conditions, such as psoriasis, eczema, and fungal infections, can increase dryness of the skin thus leading to cracks or fissures. In severe cases, cracked heels may cause bleeding. If you feel you have developed cracked heels, please visit a podiatrist for professional care and treatment.
Having dry skin is one of the many factors that can result in the formation of cracked heels. Those who have biomechanical issues that increase the pressure put on the heel, may be more likely to experience cracked heels. Being obese can also create an increase in pressure put on the heels, as the feet are responsible to carry the extra weight. This causes a loss of suppleness in the pads of the feet. Due to this lack of flexibility and increased pressure, cracks and deep fissures can form on the heels. Wearing open back shoes can also be a risk factor for developing cracked heels, as these types of shoes may cause the fat pads in the heel to expand sideways, creating cracks. Certain skin conditions, such as psoriasis, eczema, and fungal infections, can increase dryness of the skin thus leading to cracks or fissures. In severe cases, cracked heels may cause bleeding. If you feel you have developed cracked heels, please visit a podiatrist for professional care and treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Brian D. Jackson, DPM from Neuhaus Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic and treatment technologies for all your foot care needs.